This story was co-published with Slate.
Introduction
PORT BYRON, New York — Six weeks before Chris Johnson was born in 1974, the U.S. government issued a warning about a substance that would nearly kill him 30 years later.
The substance was silica, a component of rock and sand that is the scourge of miners, sandblasters and other workers who breathe it in. When pulverized into dust, it can cause silicosis — a scarring of the lungs that leads to slow suffocation — as well as lung cancer.
This was no newly discovered hazard. The ancient Greeks and Romans were mindful of it. Labor Secretary Frances Perkins launched a national campaign against it in the 1930s after the knifelike particles dispatched hundreds of tunnel workers in West Virginia.
The 1974 warning by the National Institute for Occupational Safety and Health said the workplace exposure limit for silica put people in danger. NIOSH urged the U.S. Department of Labor’s Occupational Safety and Health Administration to cut the limit in half.
OSHA finally did so in 1989, only to see its work undone by a court decision. It didn’t try again until 2011. In the interim, Johnson became a bricklayer and developed acute silicosis after a five-month job that enshrouded him in dust. He’s 40 and, on paper, can expect to survive less than five years.
As Johnson’s experience shows, inaction has consequences. Silica — which OSHA says threatens 2.2 million workers, mostly in construction — is a striking example of the government’s failure to properly regulate toxic substances in American workplaces. The silica rule still isn’t finished. If it is enacted despite industry protests, it will be only the 37th health standard issued by the agency in its 44-year history.
It’s an ignominious record given the human and economic costs of work-related disease in the United States. According to a widely cited University of California, Davis, study, an estimated 53,000 people died in 2007 from on-the-job exposures — outnumbering those killed in suicides, motor vehicle accidents, falls or homicides. More than 400,000 others got sick. The price tag: an estimated $58 billion. OSHA puts the annual toll at more than 50,000 deaths and 190,000 illnesses.
An 18-month investigation by the Center for Public Integrity has found that the epidemic of occupational disease in America isn’t merely the product of neglect or misconduct by employers. It’s the predictable result of a bifurcated system of hazard regulation — one for the general public and another, far weaker, for workers. Risks of cancer and other illnesses considered acceptable at a workplace wouldn’t be tolerated outside of it.
For years, the best OSHA has been able to do is set chemical limits so that no more than one extra cancer case would be expected among every 1,000 workers exposed at the legal maximum over their entire careers. The U.S. Environmental Protection Agency’s standards for the public are 10 to 1,000 times more protective. The real gap is often worse, a former OSHA official says.
“I can’t see any justification for treating people that differently,” said Adam M. Finkel, who heads the Penn Program on Regulation at the University of Pennsylvania Law School and was director of health standards programs at OSHA from 1995 to 2000.
• Most of OSHA’s 470 chemical exposure limits are, by the agency’s own admission, grossly outdated and don’t protect workers from a variety of ailments. Cancer, for instance: The agency’s own analyses of 16 substances estimate that cancer risks associated with legal exposures to workers over their careers are as high as six in 10. Analyses of an additional 31 exposure limits by the Center and Finkel found cancer risks above 1 in 10 for nearly half of the chemicals.
Among the Center’s findings:
• The vast majority of the tens of thousands of chemicals made or used in the U.S., including some very common and toxic substances, have no workplace exposure limits. The lung-ravaging food flavoring diacetyl. The widely used herbicide glyphosate, recently named a probable carcinogen by the World Health Organization. The agents in chemotherapy drugs, hazardous to the health care workers preparing and handling them.
• Even apparent success stories — rare cases in which chemical limits were tightened — can be Pyrrhic victories. OSHA’s own calculations suggest, for example, that the cancer risk for hexavalent chromium, a metal used in specialty paints and coatings, was as high as one in three at the limit in effect from 1971 to 2006. At the current, stricter standard, the risk is still as high as one in 22, OSHA acknowledges.
• Sampling for chemicals has fallen over the last three decades as workplaces multiplied but OSHA’s staff levels stagnated. Even so, OSHA still finds exposures above legal limits, a Center analysis found. One in six samples containing hexavalent chromium, taken after the 2006 rule change, topped the limit of 5 micrograms per cubic meter of air. Samples containing lead, a brain-damaging metal that can accumulate on a worker’s clothing and hurt the whole family, have exceeded the limit 40 percent of the time since 1984.
• NIOSH last did a nationwide workplace exposure survey more than three decades ago because it has not had the funding to update it. Critical information on both old and emerging chemical hazards across industries is missing, putting regulators and researchers at a disadvantage.
A profound toll
Job-related illness is a slow-motion tragedy few seem to understand or acknowledge. Its victims usually die one by one, out of public view, though disease clusters emerge on occasion.
More than 50 cases of bladder cancer, for example, have been tied to a small Goodyear chemical plant in Niagara Falls, New York, far above the expected number in the general population. NIOSH investigators identified the suspect chemical years ago: ortho-toluidine, used to keep tires from cracking. Exposures in the plant weren’t extreme; in fact, they were “well below” the legal limit, the investigators reported.
Goodyear, which made changes to its factory after the problem came to light, said in a statement that all but one of the 54 bladder-cancer cases identified through its own screening program involved workers who came to the plant before 1990.
“While the ortho-toluidine exposure levels in the plant have generally been far below the permissible exposure limits, engineering controls were put in place in the 1980s to further reduce levels in the plant,” the company said.
Steve Wodka, a lawyer in New Jersey who represented about half the Goodyear victims in claims settled out of court, said he knows of 62 bladder cancer cases from the plant. He calls that cluster “probably the best example of the inadequacy of the system.”
Ortho-toluidine is in a family of chemicals — aromatic amines — known since the 1930s to cause bladder cancer, Wodka said. Yet its exposure limit of 5 parts per million, adopted by OSHA in 1971, was fashioned only to protect workers from the chemical’s acute effects, not cancer.
“It remains the law of the land today,” Wodka said.
The blight of disease contracted on the job isn’t confined to factory workers. It consumes hairdressers, grocery store meat-wrappers, scientists and people in a variety of other professions. Many are stricken by middle age.
The panoply of illnesses, from nerve damage to dementia to virulent cancers, takes a profound toll on workers and their families. Careers are lost, finances shredded, marriages tested. In some cases, workers opt for macabre, last-ditch procedures to try to save their lives.
“They basically clean you out like a fish,” cancer victim Mike Dennen, who worked in asbestos-contaminated textile factories, said of his 2013 surgery. “They tell you before surgery you can end up without a bladder, you can end up without your intestines.”
Federal regulators are overwhelmed by the scope of the problem, which didn’t materialize by chance. Congress has exacerbated the situation by refusing to fortify the weak 1970 law specifying what OSHA can do. Trade groups have challenged health standards in court while workers lose their lives. The White House’s Office of Management and Budget is a vortex that sucks in proposed agency rules and doesn’t spit them out for months — or years.
David Michaels, head of OSHA since 2009, speaks frankly about the results.

Jamie Smith Hopkins/Center for Public Integrity
“With a few exceptions, OSHA’s standards to protect workers from chemical exposures are weak and out of date, or simply non-existent,” he said in a recent interview.
He cited as an example the solvent hexane, which can wreck the nervous system. OSHA’s exposure limit for the chemical is 500 parts per million, 10 times the level NIOSH says is safe.
“We know workers get sick at levels below 500 parts per million,” Michaels said. “We can’t do anything about that.”
OSHA’s exposure limits almost all date to its founding in 1971, he noted, when the agency adopted 1960s-era voluntary numbers embraced by industry. Few have been updated since, and only those few became full standards with specific technological and medical requirements.
“The law under which OSHA operates … forces us to go through a very, very complex, onerous process for regulating any individual chemical,” Michaels said. “It takes many years and millions of dollars in studies to issue one standard. And that’s why we’ve got only a few dozen standards.”
An ancient hazard
Silicosis and other dust-related diseases, the 1974 NIOSH document reported, “have probably existed since man began to dig into the earth’s crust.” Silica was a cruelly efficient killer of stone-cutters in the 17th century; slicing through the workers’ lungs during necropsy was “like cutting a mass of sand,” a Dutch physician reported in 1672. It silenced 19th-century sandstone masons in England long before they reached old age.
Silica also precipitated America’s worst industrial disaster: the deaths of more than 750 workers — many African-American — who drilled a water-diversion tunnel through silica-rich rock near Gauley Bridge, West Virginia, in the early 1930s. Death estimates reached as high as 2,000, but the full count will never be known. Sick workers were booted out of company housing. Some who died on site were carted off to unmarked graves.
Four decades after that, in December 1974, Christopher Scott Johnson was born in Auburn, New York. His life almost perfectly tracks silica’s tortured regulatory history.
The U.S. government knew about the hazards of workplace exposure to silica before Chris Johnson was born. Yet 30 years later it nearly killed him.
Chris Johnson’s life
Regulation of silica
-
OSHA adopts current standard for workplace exposure to silica
-
Dec. 1
Born in Auburn, N.Y.
-
Oct. 15
NIOSH evaluates silica as a workplace hazard and recommends to OSHA that exposure limit be cut in half
-
December
OSHA publishes advanced notice of proposed rulemaking based on NIOSH recommendation
-
June
International Agency for Research on Cancer (IARC) finds limited evidence that silica is carcinogenic to humans
-
OSHA includes stricter silica limit in sweeping revision of hundreds of air contaminants. NIOSH recommends in comments that silica be considered a potential carcinogen
-
U.S. National Toxicology Program concludes that silica is “reasonably anticipated as a human carcinogen”
-
July 7
U.S. Court of Appeals vacates 1989 air contaminants rule for general industry. OSHA is forced to revert to the old exposure limits
-
August
NIOSH issues an alert stating blasting sand containing silica can cause serious or fatal respiratory disease, citing 99 known cases of silicosis in sandblasters
-
June
Graduates from Union Springs Central High School and begins masonry career on a construction job in Utica, N.Y.
-
OSHA deems rulemaking for silica exposure a priority
-
August
OSHA launches a Special Emphasis Program on silica to reduce worker exposures through enforcement
-
October
IARC concludes silica is a human carcinogen
-
March
National Conference to Eliminate Silicosis draws some 650 participants
-
October
OSHA puts silica on its regulatory agenda
-
November
OSHA moves to pre-rule stage on silica
-
National Toxicology Program reevaluates evidence and concludes silica is “known to be a human carcinogen”
-
American Conference of Governmental Industrial Hygienists (ACGIH) lowers threshold limit value (TLV) for silica to 0.05 mg/m3, the same number recommended by NIOSH in 1974
-
Bush administration designates adoption of a new silica standard a high priority
-
OSHA identifies high rates of noncompliance with silica exposure limit, particularly in construction
-
April-September
Helps repair a brick public housing complex in Rome, N.Y.; grows short of breath toward end of job
-
Dec. 7
Admitted to Strong Memorial Hospital in Rochester, N.Y., and diagnosed with acute silicosis
-
Dec. 15
Left lung lavage
-
Dec. 28
Released from hospital
-
Feb. 12
Marries Beverly Johnson
-
May 16
Bilateral lung lavage
-
Files lawsuit against the Rome Housing Authority
-
No longer needs a constant external oxygen supply
-
ACGIH lowers TLV for silica to 0.025 mg/m3
-
Jan. 24
OSHA implements a National Emphasis Program for silica
-
Obama administration designates silica standard a high priority
-
Lawsuit is settled
-
Feb. 14
Proposed silica rule submitted to Office of Management and Budget for supposed 90-day review
-
March-August
Nine meetings on silica are held at OMB; industry representatives outnumber labor and public-health representatives 44-to-13 at these meetings
-
March
Two more meetings are held at OMB; industry representatives outnumber labor and public-health representatives 9-to-1
-
Aug. 23
After 921 days, OMB completes proposed rule to set permissible exposure limit to .05 mg/m3 – the same number recommended by NIOSH nearly 40 years earlier
-
March 18
OSHA holds public hearings on the proposed rule
-
June
Tries to return to masonry, has to leave after a few weeks due to health
-
Feb. 13
Centers for Disease Control and Prevention reports that 1,437 people had silicosis listed as an underlying or contributing cause of death between 2001 and 2010, and that 2 million American workers remain potentially exposed to silica
-
March 23
The Construction Industry Safety Coalition, an industry group, submits report to OSHA claiming silica rule could cost the construction industry more than $4.9 billion a year and lead to more than 52,700 lost jobs. OSHA estimates $511 million in annual costs
The month of Johnson’s birth, OSHA published an “advance notice of proposed rulemaking,” indicating movement toward a new silica standard. That effort fizzled due to a lack of funds, according to the head of OSHA at the time.
Silica-related death and disease continued. As bad as things were in foundries and other dusty, fixed establishments, where workers legally could be exposed to twice the NIOSH-recommended silica limit, construction was far worse. Employers in that sector could subject workers to five times the recommended limit without breaking the law.
That’s still the case.
Johnson landed in the construction category in 1993. He became a bricklayer, also known as a mason, following in the footsteps of two uncles. He crafted sidewalks and floors with bricks and stone, and helped repair and put up buildings.

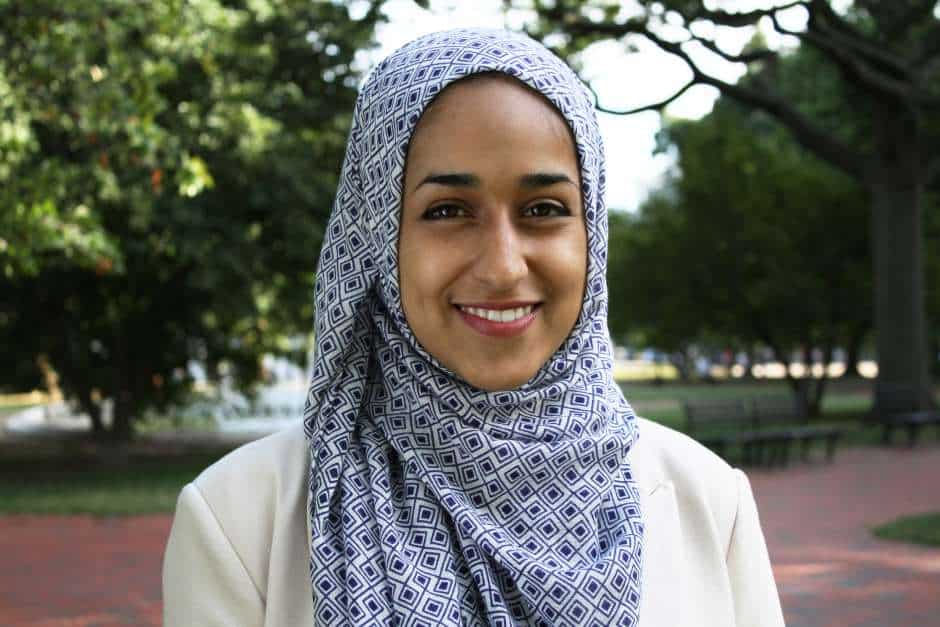
Maryam Jameel/Center for Public Integrity
“I was very happy with my job,” he said in an interview at his home in Port Byron, west of Syracuse. “I felt fulfillment.”
Johnson said he was oblivious to silica’s destructive properties. That didn’t matter until he was assigned a job in Rome, New York, in April 2004. Standing on hydraulic lifts, Johnson and his co-workers at a small contracting firm removed and replaced damaged brick from the façades of three apartment buildings operated by the Rome Housing Authority.
The work, which lasted through September of that year, generated “a tremendous amount of dust,” Johnson said. “You’re in a basket that’s maybe six feet wide and two or three feet deep, so you’re pretty much stuck right there.”
The workers were given disposable paper masks, known by experts to be ineffective against microscopic silica particles. The one half-face respirator on the job had a broken strap, “so we didn’t really use it,” Johnson said.
They had tools to suppress the dust: Their diamond-bladed, 14-inch demolition saws came equipped with hose attachments for “wet cutting.” But the project manager for the housing authority refused to allow the practice, fearing it would “make too much of a mess,” according to an affidavit given by a former co-worker in a lawsuit Johnson later filed against the authority. OSHA rules, moreover, don’t require it.
Johnson did “about 90% of the saw cutting and grinding on the job,” his former colleague said in the affidavit. “In fact, he was often so covered in dust we nicknamed him ‘Dusty.’”
Jim Baldwin, who joined the housing authority as executive director years later, said he would have allowed wet cutting “because of the danger caused by the inhalation of the fine dust.”
“Not having proper respirators on the job was certainly a factor in the worker’s illness,” he added by email. “For that I would have shut the job down until that equipment was made available and was being used.”
There is no way to know how much silica Johnson inhaled. But the current rule for construction is so weak, even employers that stay within the legal limit can be “sentencing someone to death from lung disease,” said Celeste Monforton, a lecturer at George Washington University and a former Labor Department analyst and adviser.
By the time the Rome job ended, “something was not right with me,” Johnson said. He was short of breath, losing weight rapidly, unable to do simple tasks without exertion. “I had no clue what was going on.”
The answer came early in a three-week stay at the University of Rochester’s Strong Memorial Hospital in December 2004. Johnson’s parents drove him there after his right lung collapsed following a biopsy, and further tests showed he had acute silicosis triggered by mixed dust exposure.
He underwent an unusual procedure called a lavage, in which his lung was flushed of sticky material filling up the air sacs and robbing him of oxygen. He stayed on a ventilator for nine days.
“None of the doctors really even knew if he was going to pull through or not,” said his wife, Beverly.

The procedure didn’t help much. Johnson continued to struggle for air as he rested fitfully at home in early 2005. He was a candidate for a double lung transplant, a prospect he found unappealing once he learned the odds of survival: less than half of patients would live five years, and less than a quarter would survive 10.
He opted instead for a second lavage at the Cleveland Clinic in May 2005. This one took. By 2006 his lung disease had stabilized, though it hadn’t been cured.
Internist and lung specialist Dr. William Beckett treated Johnson in Rochester and was so struck by the severity of the young mason’s condition that he co-authored an article about it for a medical journal. In an interview, he noted the banality of the substance that had gummed up Johnson’s lungs.
“This is not an unusual material. It’s not exotic,” Beckett, now affiliated with Harvard Medical School and Mount Auburn Hospital in Cambridge, Massachusetts, said of silica. “It’s something that everybody is around, but the people who cut through it or work with it are susceptible to getting disease from it.”
Beckett chaired an American Thoracic Society committee that called for a stricter OSHA silica limit in 1997. To his dismay, the old one is still in place.
“There are many, many, I’m sure, young men in the United States who are doing the same kind of job [Johnson did],” he said, “and probably getting the same kinds of exposures.”
Forty years of futility
OSHA’s 40-years-and-counting quest to keep silica from killing workers is a study in inertia and frustration. The agency tried to tighten exposure limits for silica and 375 other substances in a 1989 rule, but a federal appeals court struck it down, saying the analyses OSHA used to justify the rule weren’t detailed enough.
It took OSHA nearly two decades to regroup, even though it deemed silica a regulatory priority in 1995 and 2002. In the meantime, evidence hardened that silica could cause lung cancer in addition to silicosis.
It’s unlikely any group of workers has felt the sting of lax silica controls more than sandblasters, who use pressurized guns to shoot sand at corroded surfaces to prepare them for painting. The sand breaks apart as it strikes metal, creating clouds of dust laced with invisible shards of quartz that scar the lungs.
NIOSH, noting available alternatives such as nut shells and sawdust, suggested in 1974 that sandblasting with silica be banned. Britain and a swath of mainland Europe had already done so by that point.
But industry groups in the United States, like the euphemistically named Silica Safety Association, composed of purveyors and beneficiaries of sandblasting, lobbied successfully in the 1970s to fend off a ban, predicting economic hardship.
In February 2011, OSHA finally sent a proposed silica rule to the Office of Management and Budget for vetting. It emerged 921 days later in 2013. OMB officials will not say why it took so long; 90 days, plus a single 30-day extension, is supposed to be the maximum unless the rulemaking agency asks for more time.
Apart from trimming the silica exposure limit to the NIOSH-recommended number for all workers, the proposed standard would require employers to control dust with methods such as water or vacuum systems and provide medical monitoring for highly exposed workers. OSHA predicted it would save nearly 700 lives and prevent 1,600 new cases of silicosis per year.
The Labor Department held 14 days of hearings in Washington, D.C., in the spring of 2014. Among the witnesses was construction worker Santiago Hernandez, who’d come to the United States five years earlier from Tlaxcala, Mexico, expecting to find safer conditions.





Join the conversation
Show Comments