Introduction
Our data analysis behind the Unequal Risk investigation into work-related diseases in America.
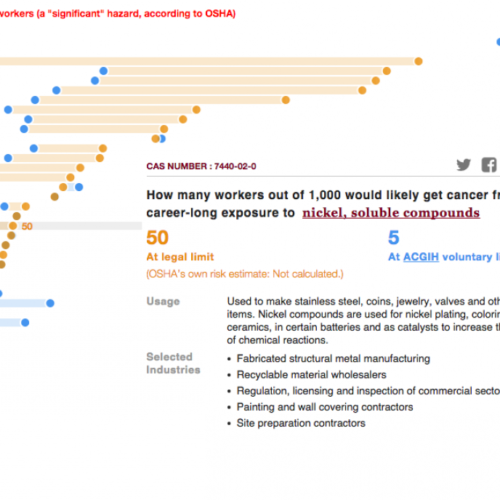
CANCER RISK
Our interactive cancer-risk graphic is based on an analysis by Adam M. Finkel — a former director of OSHA’s health regulatory divisions who is now at the University of Pennsylvania Law School — and the Center for Public Integrity. It tackles a thorny question: If 1,000 workers are exposed to a chemical’s legal limit over their entire careers, how many will likely get cancer as a result of that exposure? What, in other words, is the excess risk above and beyond the cancer risk everyone faces?
First, an important note: Any risk analysis produces estimates, not exact numbers. Its value is showing how much hazards can vary under the law. (This analysis doesn’t look at average exposures, but rather the impact of what exposure at exactly the legal limit would be. But the Center also mined an OSHA inspections database for a separate analysis to find out how often the agency detected several toxic substances above the legal level. See the exposure-data section below for more on that.)
Our group of theoretical workers is 1,000-strong for a reason. OSHA considers a grave risk such as cancer that affects one worker in 1,000, all equally exposed over the length of their careers, to be “clearly significant.”
That means the agency should enact workplace standards that lead to less risk, particularly since OSHA says it doesn’t see 1 in 1,000 as the dividing line between too much and OK. But for all the years the agency has quantified risk — since the Supreme Court required it in 1980 — OSHA has never enacted a standard on the right side of that threshold, it says. Court decisions have made clear that limits must be set based on what is technologically and economically feasible — a hotly contested issue.
Americans enjoy much stronger federal protections from chemicals when they’re off the clock than on it. The U.S. Environmental Protection Agency, operating under different laws and court decisions, aims to protect the public so no more than one cancer case in 10,000 results from pollution in the community — and more often, no more than one in 1 million. On paper, that’s 10 to 1,000 times more protective.
What our analysis with Finkel suggests is that the actual difference is far worse. That’s because cancer risks at OSHA’s exposure limits are often much higher than 1 in 1,000.
The analysis relied on cancer-risk figures developed by the U.S. EPA and California’s EPA for certain known or likely human carcinogens. These “inhalation unit risk” figures allow researchers to calculate cancer risk over a lifetime of community exposure at a specified level. We adjusted these figures to account for on-the-job exposure: 40 years instead of 70, 50 weeks a year instead of 52, five days a week instead of seven and the amount of air inhaled by the typical employee during a workday compared with a resident off work all day (10 cubic meters of air vs. 20, which takes into account both the difference in hours and breathing rates).
We used U.S. EPA risk figures when available, and if not, CalEPA. After adjusting the figures for occupational exposure, we used them to calculate the risk at OSHA limits as well as the risk at voluntary guidelines called “Threshold Limit Values.” TLVs, as they’re known, are developed by the nonprofit American Conference of Governmental Industrial Hygienists and are often tighter than OSHA’s “Permissible Exposure Limits.”
OSHA, in fact, recommends that companies look to voluntary limits such as the TLVs rather than its own standards to protect workers. In 2013 the agency released a side-by-side comparison to make that easier: OSHA limits vs. TLVs, the National Institute for Occupational Safety and Health’s guidelines and California’s workplace limits, which are mandated only in that state. (California is one of the few states that sets its own exposure limits.)
Our analysis relied on that side-by-side comparison for information on OSHA limits and the ACGIH’s TLVs. The vast majority of OSHA’s limits are actually decades-old TLVs, adopted by the then-new agency in 1971. While the ACGIH has kept updating since, most of OSHA’s limits haven’t changed. (Why? More on that here and here.)
Finkel developed the initial analysis that estimated the cancer risks at OSHA limits and TLVs. He shared that with us and advised us as we fact-checked the underlying figures, pulled in California data and tweaked the method with input from him and other experts.
California conducted an analysis similar to ours in 2007 when it looked at workplace health hazards at legal exposure limits. Julia Quint, who launched and co-managed the project before retiring from the California Department of Public Health, was among the experts who reviewed a sample of our analysis. She said it is consistent with California’s method, which that state uses as it considers tighter exposure limits.
For some substances, OSHA has produced its own cancer risk estimates. In those cases, we show the agency estimate alongside our calculations. Sometimes they’re about the same; in other cases, they’re far apart. OSHA calculates risk based on a 45-year career rather than a 40-year one, which explains some differences. In addition, the agency’s assessments delve more fully into risk quantification, particularly the specific way a substance’s risk varies as exposure levels change. On the other hand, most of OSHA’s estimates are more than two decades old, so the science underpinning them can be out of date.
OSHA’s calculation for o-toluidine, as an example, is from the 1980s and suggests the exposure limit (unchanged since 1971) carries far less risk than one cancer case in 1,000. But the National Institute for Occupational Safety and Health, or NIOSH, later implicated the chemical in a cluster of bladder-cancer cases among workers at one plant — people exposed to levels well below the legal limit. The inhalation risk figure California’s EPA produced in 1992 suggests the cancer risk at OSHA’s workplace limit is 197 in 1,000, nearly two in 10.
The country needs modern, full-blown risk assessments for workplace chemicals, said Andrew Maier, an occupational toxicology and risk assessment scientist who is an associate professor at the University of Cincinnati College of Medicine. The method we used for our analysis is likely to produce “upper-bound” estimates, he said, but he considers it a useful approach to prioritize the chemicals “that need the most attention.”
Finkel, who has a doctorate in environmental health sciences and has worked on the cutting edge of risk assessment for more than 30 years, said there’s been a “raging debate” that entire time about whether risk estimates such as the EPA’s are really at the upper end of the spectrum, and if so, how much. He says there’s underestimation issues at work, too, and he believes risk is much less likely to be overstated when exposures are higher — like at OSHA’s legal limits.
Quint, for her part, thinks OSHA should take a page from California’s book and convert the risk work the EPA has already done so it’s relevant for workers.
“OSHA, frankly, does not have the personnel … to do detailed risk assessments for each one of these chemicals that need to be assessed,” said Quint, a toxicologist. “You don’t have to repeat all that work. You can use existing information, tweaked as we do for occupational health.”
Not included in our analysis: Risks from carcinogens that don’t have EPA or CalEPA risk factors. Non-cancer risks aren’t accounted for, either. Many substances, such as beryllium, can cause other types of diseases that are serious or even lethal.
We wish we had more comprehensive details about the chemicals’ uses, including all the sectors and industries where exposures occur. Such information is spotty. (One frequently cited source is NIOSH’s survey of workplace exposures — from three decades ago. The agency says it has not had the funding for an update.)
We relied on information from the Agency for Toxic Substances and Disease Registry, the EPA and other government sources, including the New Jersey Department of Health, to explain how chemicals are used and to give insight into which sectors (such as manufacturing or construction) come into contact with them. But much of the sector information, and all of the detailed industry information, came from a Center analysis of OSHA sampling data taken by inspectors at workplaces.
That’s a limited snapshot: OSHA can sample at only a fraction of workplaces. But the sampling results offer details we couldn’t find anywhere else. We looked at chemicals detected from 2000 to 2013 and, in cases where a substance was found in more than five different industries, included a varied selection in our graphic.
We also analyzed the sampling data for a separate look at overexposures. Read on for details about that.
EXPOSURE DATA
When OSHA conducts health inspections at workplaces, investigators can sample the air for potentially dangerous substances. All the samples collected by federal inspectors, and some of those taken by state OSHA inspectors, are analyzed at OSHA’s lab near Salt Lake City.
OSHA made a database of those samples, dating back to 1984, available online after Finkel — the former OSHA official — won a lawsuit in 2007 to get the agency to release it.
We analyzed the database through 2013 to see how often the levels of certain substances topped legal limits. Why not all substances? Because there’s no handy “over the limit” data point. You need to find the limits yourself and delve into their history to see if they were once looser. The samples also require work before comparison is possible. (More on that in a moment.) We ultimately looked at several chemicals and metals that are well-known hazards, including lead and formaldehyde.
Our analysis focused on the types of samples that characterize potential inhalation exposures: “personal” samples — air grabbed by sampling devices attached to workers — and “area” samples that measure air in a workspace where multiple people might labor.
We knew we couldn’t find out what the average U.S. worker, or even the average worker in a select industry, gets exposed to. That’s because OSHA doesn’t have nearly enough staff to sample every workplace. If federal OSHA inspectors were to try, the AFL-CIO calculated this spring, it would take 140 years to get to each workplace under their jurisdiction a single time.
So the samples are, quite literally, a sample. And they’re not a random one, because inspections can be launched by complaints, accidents and OSHA’s determinations about which industries or employers are high-hazard, not only by chance selection.
So instead, we asked an answerable question: When samples test positive for a substance — the lab’s equipment detects it — how often do levels exceed legal limits? We also wondered how sample results would compare with exposure recommendations from the National Institute for Occupational Safety and Health, often tighter than OSHA’s hard-to-update limits.
But, as OSHA’s Salt Lake City experts explained, you can’t simply compare sample results to the agency’s limits. That’s because inspectors will often change sampling devices on workers through the day, so a single worker might produce two, three or more samples that together represent a full workday. You need to combine all the related samples to compare to OSHA’s eight-hour-average limits. (How? Multiply the individual samples’ results by the amount of time sampled, add the related ones together — they have a unique ID — and then divide by 480, the minutes in an eight-hour day.)
The Salt Lake technical staff walked us through those steps and looked at key results to check that we hadn’t tripped ourselves up. We appreciate their patient assistance.
You can see our results in several places: hexavalent chromium and lead in this story, mercury vapors in this piece and formaldehyde in this list of eye-popping facts. Lead was striking because samples, taken at workplaces ranging from construction sites to foundries to indoor shooting ranges, frequently exceeded the legal limit. Formaldehyde samples, by contrast, rarely did — but most with detectable levels topped the amount NIOSH recommends employers not exceed.
Side note: OSHA enacted stricter industry-wide limits for two of the substances after 1984. That puts them among the relatively few changed since the agency adopted its thresholds in 1971, a sign of how very well-established the dangers are. We looked at samples for the relevant years: 2006 onward for hexavalent chromium (OSHA’s most recently tightened exposure limit), and 1988 onward for formaldehyde.
The lead limit for most industries was set in 1978, but an exception was made for construction until mid-1993, when that sector’s limit was brought in line with the one for other businesses. We analyzed lead samples for 1984-2013, with construction firms compared to their looser limit, as well as 1994-2013 and found approximately the same percentage of overexposures for both periods.
Read more in Inequality, Opportunity and Poverty
Unequal Risk
Some paint strippers are killing people. The EPA promised to act — but hasn’t.
For now, the only ones yanking methylene chloride paint removers off the shelves are retailers.
Join the conversation
Show Comments