Introduction
Sandy Guest, 55, hairdresser

Sandy Guest “loved doing hair,” her daughter says.
Guest worked at salons in Southern California, mostly Orange County. “She always said that she loved making people feel great, that it wasn’t work for her,” said Guest’s daughter, Adrianne Matheney.
Most of the time, Guest bought her supplies from the salon owners. Among those products was a hair-straightening line called Brazilian Blowout.
Brazilian Blowout, as it happened, was loaded with formaldehyde, a carcinogen. Separate investigations by Oregon and California officials found the chemical “well above regulated levels” in the product, despite owner GIB LLC’s claims that it was formaldehyde-free.
Guest knew none of this when she used it on customers’ hair. Described by her daughter as a “workhorse” who regularly put in 12- to 14-hour days, she grew pale and tired in 2011. She was diagnosed with myelodysplastic syndrome, or MDS, a condition also known as pre-leukemia. After chemotherapy and a bone marrow transplant, she developed acute myelogenous leukemia.
“Getting the bone marrow transplant — that’s what knocked her down. That was horrific,” said Matheney, of San Clemente. “It was terribly painful.”
Guest died at 55 on April 16, 2013.
A variety of salon products can be hazardous, according to a November report from environmental-health group Women’s Voices for the Earth. Ingredients in haircare and nail supplies have been linked to cancer, respiratory problems, birth defects and other health ailments, the report said. The National Institute for Occupational Safety and Health has also cautioned workers about beauty-industry chemical exposures.
Guest’s lawyer, Kimberly Miller, has had several other clients who worked in salons and developed cancer. (Guest sued a variety of product manufacturers a year before her death; Miller said she could not discuss the case’s resolution.)
The packaging of beauty supplies, of the sort Guest used, is “intended to obscure the potent chemicals and carcinogens that can be found in some products,” Miller said.
Brazilian Blowout is among the most high-profile because it was popular and specifically advertised as having no formaldehyde. Warnings about it mounted from state and federal officials after stylists complained of nosebleeds, respiratory problems and other symptoms. A California attorney general’s settlement with GIB in 2012 required the company to pay $600,000, alert consumers about the risks and cease “deceptive advertising” of Brazilian Blowout Acai Smoothing Solution and Brazilian Blowout Professional Smoothing Solution “as formaldehyde-free and safe.”
GIB — which does business as Brazilian Blowout — pushed back against regulators at first. When the Oregon Occupational Safety and Health Division announced its testing results in 2010, GIB insisted in a statement that its products were formaldehyde-free and said “there is no reason to believe that the formulation tested” was actually Brazilian Blowout. The company filed, and later dropped, a lawsuit against the state.
GIB did not respond to requests for comment. But in 2012, after the settlement with California, CEO Michael Brady told The New York Times that Brazilian Blowout is safe if properly used in an area with good ventilation.
“We just want people to treat it like they do aspirin — make sure you only use it as directed,” he said.
Many hair salons don’t have the ventilation systems they would need to work with formaldehyde-emitting products, warned the lead author of a 2013 University of California, Berkeley, study that measured Brazilian Blowout exposure levels.
Brazilian Blowout remains on the market. There’s now a “Zero+” formulation the company advertises as having “0% Formaldehyde released before, during or after the treatment”; another option is “Brazilian Blowout Original.”
Matheney said she was “angry and shocked” to learn that the product might have sickened her mother, with whom she was very close.
“Mom said if she had known [the risks], she never would have used those products,” Matheney said. “Here she was, trying to make other people feel beautiful, and this is what happens.”
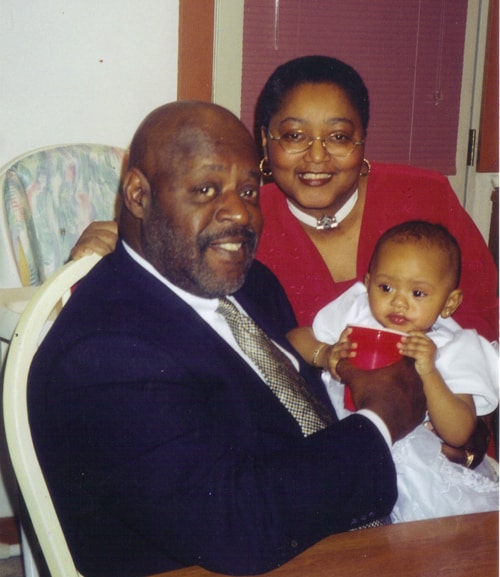
Ricardo Corona, 46, food-flavoring production worker
Ricardo Corona would come home smelling of chocolate, vanilla or strawberries. He spent his days working for Carmi Flavor & Fragrance Co. in Los Angeles County, mixing pungently scented powders and liquids to create food flavorings.

“You get a little headache when you go in there,” Corona said. His skin would itch through his latex gloves, and his eyes grew red behind safety goggles as he measured and stirred. When he asked if the substances could be harmful, his supervisor reassured him that a paper mask would protect his lungs: “As long as we had the mask, we were good.”
Corona started the job in February 2006. By May, he was seeing a doctor for severe breathing problems. He was prescribed medicine for bronchitis, but his condition deteriorated. He no longer had the energy to play with his two children or exercise at the gym.
“I would go to my mom’s house, and I couldn’t move from the couch,” Corona said. He would rest until it was time to go to work again.
One of the main chemicals Corona handled was diacetyl, a common ingredient in butter flavorings and a known cause of lung disease. Diacetyl, like many substances used in flavoring manufacturing, does not have a workplace exposure limit set by the Occupational Safety and Health Administration.
Corona’s coughing and wheezing worsened. He and some of his co-workers, also suffering, didn’t have the energy to finish tasks like grocery shopping. “We would just leave our carts there and have to go home, or somebody had to pick us up, because we couldn’t breathe anymore,” he said.
Corona and two other workers at the facility sued various diacetyl manufacturers and suppliers, eventually settling out of court. Carmi Flavors was not named in the suit.
Diacetyl’s harmful effects were known years before Corona encountered the chemical. In 2000, the National Institute for Occupational Safety and Health investigated a popcorn manufacturing plant after eight of its workers became ill. In 2003, NIOSH issued an alert saying that breathing diacetyl and other flavoring chemicals may lead to severe lung disease.
The president and CEO of Carmi Flavors, Eliot Carmi, said the company stopped using diacetyl in 2007. “We had no knowledge of its potential, and we eliminated it when we found out,” he said.
Corona had taken the job at Carmi as a “stepping stone” to a career in a different field or higher-paying work. In June, he had his eyes on a job with the California Department of Transportation. But to get it he had to pass a physical examination, and his lungs held him back.
“My stepping stone broke right under my foot,” he said.
In July 2006, just weeks after Corona’s 38th birthday, doctors diagnosed a progressive and irreversible disease called bronchiolitis obliterans. The smallest airways of his lungs were scarred, blocking the movement of air. He was put on a waiting list for a lung transplant.
Over the next two years, his sister took him to and from hospitals. Sometimes he required round-the-clock oxygen from a tank. Once, he passed out in a restroom and his rescuers had to break down a door to get to him.
He was scared, angry and depressed.
But his illness indirectly brought him one gift. During a hospital visit, he ran into a former girlfriend, and they rekindled their relationship. Shortly after he received a lung transplant in 2009, the two were married.
At his home in Whittier, California, the 46-year-old Corona takes more than 60 pills a day. Declared 99-percent disabled, he hasn’t held a job since he worked at Carmi but has seen improvement in his health.
“There’s a lot of things I can’t do, but there’s a lot of things I’m grateful to do,” he said.
Exercising. Playing with his granddaughter. And simply walking and breathing — two functions he couldn’t take for granted just a few years ago.
Frank Lipari, 60, research scientist
Frank Lipari spent his career in an automotive research lab, working on experiments with chemicals. The chemicals, in turn, were working on him.

He inhaled them daily in his combined laboratory-office. He also inhaled colleagues’ chemicals, said his wife, Nancy, because his lab was the designated storage area and dumping spot. For 23 years, he came to work and breathed that air until his body could take no more.
Frank, a research scientist for General Motors’ technical center in Warren, Michigan, went on disability retirement in 2001 at age 48 after respiratory distress so severe he mistook it for a heart attack. His health difficulties mounted — memory loss, confusion, vasculitis, neuropathy, osteoporosis, heart troubles — until he died in 2013 at age 60.
“He had practically every malady that organic solvents could cause,” said his occupational-disease specialist, Dr. Michael R. Harbut, a clinical professor of internal medicine at Wayne State University.
GM spokesman Dan Flores said in a statement that the company’s “condolences and deepest sympathies go to the family of Dr. Lipari.”
“While we cannot comment on Dr. Lipari’s specific work environment over the course of his career, we can say that GM has a strong ongoing commitment to the health and safety of our employees,” Flores said.
Laboratory work — which employs more than 500,000 people in the U.S. — can be dangerous for a variety of reasons, the Occupational Safety and Health Administration warns. Besides chemicals, lab workers can be exposed to biological agents, explosive gases and radiation. Some hazards kill quickly. Others take time.
John Newquist, a safety trainer who worked at OSHA for 30 years, worries about college labs in particular. The ventilation systems he’s seen are usually inadequate, and “they don’t sample for these exposures” to make sure students and teachers aren’t at risk from the carcinogens and other hazardous chemicals they use, he said.
“How many people are getting sick years later? We don’t know,” he said. “Nobody’s doing research on this field.”
Nancy Lipari, a registered nurse who married Frank in 2000, said he worked with carcinogens such as benzene but did not develop cancer. Instead, doctors told her the constant onslaught of multiple chemicals seemed to have kicked his immune system into overdrive, “and then his immune system just started attacking itself.”
Frank sued GM, but he wasn’t able to get over a key hurdle. Workers in Michigan must show their employer deliberately acted to injure them.
Until Frank’s death, each day brought with it the unspoken threat of some new problem. Blood pressure spiking, then plummeting. Infection after infection, the last of which precipitated his death. And once, his wife said, he rolled over in bed and broke seven ribs.
“That’s how fragile his bones were,” said Nancy, who lives in a suburb of Detroit. “The calcium leached right out.”
He lost bits of himself year by year as body and mind declined. Activities he had to give up ranged from the big — such as his work, focused on emissions reduction, and driving — to smaller but still difficult losses, like golf and paying bills. He’d forget conversations he’d had, movies he’d seen, passages in books he’d read just the day before.
But at the same time, he doggedly studied astrophysics, a subject he loved, and wrote down formulas and other information to prove he knew it, Nancy said. He made her laugh. He wasn’t bitter.
What he wished, she said, is that he’d pressed harder for safer working conditions, such as a separate office and better protective equipment. He was an easygoing man who went along with the status quo. He also didn’t have the perspective on safety procedures that can come from working in different places — GM hired him right after he earned his doctorate in analytical chemistry.
Nancy wants workers to remember her husband’s regret.
“People need to be more aware going into things what the long-term issues could be … and not to just listen to their employer saying, ‘This is the way it’s always been done,’ but to question it,” she said. “It’s too late to question when you’re already sick.”
Rick Luzaich, 62, insurance salesman whose first job was in a machine shop

Rick Luzaich took the job out of high school — two years grinding parts in a Minnesota machine shop. A career in business management and other white-collar jobs followed, his days as a grinder fading into the distance.
What he didn’t know then or for many years afterward was just what he’d inhaled during that short stint doing blue-collar work.
He was in his late 50s, living outside Minneapolis, when he began feeling short-winded and ill. Heart trouble, doctors thought at first. Last year, he and wife Jennifer found out what really ailed him: mesothelioma, an aggressive cancer triggered by exposure to asbestos.
Asbestos is a mineral that can be processed into heat-resistant fluffy fibers, an excellent insulator but hazardous to health. Companies put asbestos into all sorts of products for decades, in some cases before and in other cases after they knew the risks involved. Items ranged from widely-installed insulation to firefighters’ protective gear. Also on the list: grinding wheels.
Rick, now 62, said he beat out hundreds of candidates for that grinding job and was thrilled by the good pay.
“Little did I know that the whole time I was working there, I was killing myself,” he said.
Mesothelioma, one of several diseases asbestos can set in motion, is a cancer that takes its time. Decades can pass before symptoms appear.
Construction workers and people employed at shipyards, chemical plants and refineries have been among the worst hit in the U.S., according to the National Institute for Occupational Safety and Health, known as NIOSH. The federal government put some limits on asbestos usage in the 1970s, but the substance is not fully banned.
More than 26,000 people died of malignant mesothelioma between 2001 and 2010, according to NIOSH’s most recent tally. Annual deaths rose from 2,500 to 2,700 during that period.
Robert E. Shuttlesworth, a Houston lawyer who helped represent the Luzaichs in lawsuits against manufacturers, usually sees clients in their 60s and 70s who were exposed 40 or more years ago. Some, however, are younger. Many worked in industrial settings; others were exposed when their spouses or parents brought the often-invisible fibers home on their clothes, or when companies near them disposed of asbestos improperly.
“There’s places in Texas where they closed down the plant, they just bulldozed it, and you get these mounds of asbestos, … nothing but an asbestos hill,” Shuttlesworth said.
In cases of mesothelioma, asbestos fibers have usually damaged cells in the lining around the lungs.
“Imagine your lungs being coated in cement and not being able to be used. That’s what I have,” Rick Luzaich said. “It’s the left lung. Now, lately, just lately, it’s spread to the right lung. … Feels like you’re trying to run up the stairs breathing through a straw. That’s the feeling. And all the time — not just sometime, all the time.”
He and Jennifer, 48, married in 2007 and were an active couple, boating and exercising. That’s out of the question now. So is paid employment — dealing with mesothelioma is a full-time job for them both. Rick stopped selling insurance last year as pain and fatigue overcame him. After he endured four rounds of chemotherapy she feared would kill him, Jennifer left her job, too.
They’ve pieced some financial help together like a patchwork quilt. Rick now gets federal disability payments. The lawsuits against several manufacturers of products with asbestos were “resolved,” said another of their lawyers, Ross Stomel. And friends organized a fundraiser last year. But big, uncovered medical expenses paired with the regular costs of everyday life have left their finances in “horrible” shape, Jennifer said.
She tries to keep her spirits up. She cares for Rick. She raises her children, ages 11 and 12. She researches clinical trials and helped him enroll in two, a way to hold onto hope.
Over it all hangs a terrible question.
“Every day you wake up and wonder, how long is he going to have?” she said.
Deborah Rodgers, 62, grocery-store meat wrapper
Just the flu, the emergency-room doctor said. But Deborah Rodgers kept feeling sick — a place-specific sort of sick.
“When I was home, I was all right,” she said, “but when I came back to work, I had hoarseness in my throat.”
Going home eventually stopped working its magic. Hoarseness turned to severe laryngitis, and then the Detroit woman’s lungs started failing her. She’d developed asthma from inhaling plastic fumes during her years of wrapping meat at grocery stores — a condition so extreme that she’s had three emergency tracheotomies to help her breathe.
By 1996, at age 44, she no longer could work.
Job-triggered respiratory distress isn’t unusual. Nearly 2 million people in 22 states have asthma caused or worsened by work, the National Institute for Occupational Safety and Health estimated this year.
There’s a name for Rodgers’ specific ailment: meat wrappers’ asthma. She worked as a meat wrapper for two decades but had never heard the term before her diagnosis. She suspects that some with the condition don’t know what they have — doctors struggled to pinpoint her problem until one referred her to an occupational-disease specialist.
Rodgers cut plastic with a hot wire, and the heat is “what liberates the fumes,” said that specialist, Dr. Michael R. Harbut, a clinical professor of internal medicine at Wayne State University. Good ventilation can help, he noted, but Rodgers says she worked in a back room with no system to remove the fumes. They built up to the point that “you would think it was a smoke party” going on in there, she said.
She left grocery-store work in 1995, but her exposure triggered a heightened sensitivity to chemicals that still bedevils her. A small whiff can set off dangerous bronchospasms, in which the airways “clamp down,” Harbut said.
“She got sick wrapping up the meat, but it proliferated, if you will, so even small amounts of car exhaust or gasoline or cigarette smoke triggered the same response,” he said. “It’s sort of like if you fall on the sidewalk and scrape your arm: It hurts pretty badly, but then if you take alcohol or iodine on the wound, it hurts badly again, even though it’s a different [substance] than the sidewalk. … The same thing goes on inside the lung.”
After wrapping meat and before winning approval for federal disability payments in 1996, Rodgers tried jobs in two different fields. But she couldn’t handle the paint smell while inspecting cars for scratches or the dust at a shoe shop. She even had attacks in Harbut’s office, despite his ban on smoking and perfumes. He thinks she might have died during the worst years if not for her family’s support and expertise. Her daughter, Felicia James, became a respiratory therapist and nurse after Rodgers fell ill.
Steroids eventually brought some relief. But that came at a cost. Rodgers, 62, developed diabetes and congestive heart failure, conditions that can be triggered by steroid medications.
Even now, she must be cautious about where she goes. She can’t afford more odor-triggered attacks.
“I stay home a lot,” she said. When she does venture out, she takes her husband or her grandchildren to be safe. “They are extremely overprotective with me.”
Read more in Inequality, Opportunity and Poverty
Unequal Risk
Some paint strippers are killing people. The EPA promised to act — but hasn’t.
For now, the only ones yanking methylene chloride paint removers off the shelves are retailers.


Join the conversation
Show Comments