Introduction
Do I qualify for reduced-cost health coverage based on my income?
The 2021 federal poverty level (FPL) income numbers can determine eligibility for Medicaid and the Children’s Health Insurance Program (CHIP). FPL also determines eligibility for health insurance subsidies on Healthcare.gov and state marketplaces. Find those numbers here.
Did my state expand Medicaid under the Affordable Care Act?
It depends where you live.
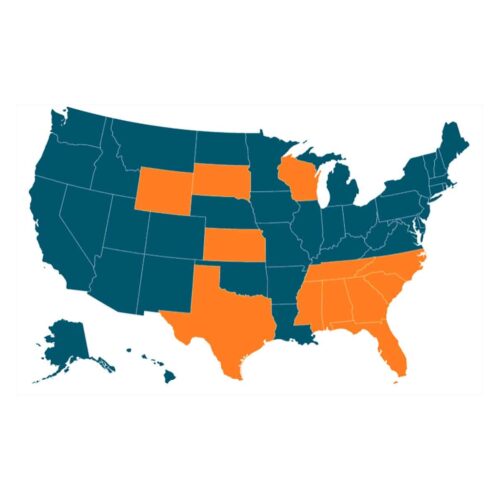
A 2012 Supreme Court decision gave all states the option to not expand Medicaid eligibility, but 12 states continue to refuse, including eight southern states. The American Rescue Plan passed earlier this year included financial incentives to encourage expansion, but those 12 still haven’t wavered.
Check the status of your state.
What happened in states that chose to expand Medicaid?
Medicaid expansion allows more low-income people living in the state to qualify for the health care program based on their income. Otherwise income eligibility rules differ between states.
Louisiana is the only state in the Deep South to have expanded coverage under the Affordable Care Act. Access to health insurance for the working poor decreased uncompensated care costs and supported the economy. And since the decision, Medicaid coverage of the state’s adult population has risen by nearly 40%.
What about states that didn’t choose to expand?
In those states, most single, childless adults remain ineligible for Medicaid coverage regardless of what they earn each year.
In Mississippi, 78% of the people who would become eligible for health insurance with expansion are poor adults without children.
Mississippi and other southern states that chose not to expand Medicaid have seen little change in the proportion of the adult population, ages 64 and younger, that has Medicaid coverage. Louisiana, though, is covering a greater share of adults.
Has Medicaid expansion helped rural hospitals facing closures?
Yes, being located in a Medicaid expansion state is often a protective factor for rural hospitals.
In April 2020, we reported that many rural hospitals have closed after years of financial struggles. Those that remain open often have fewer employees, including specialized doctors and critical care nurses.
But since the major Affordable Care Act Provisions took hold in 2014, charity care and bad debt have fallen among hospitals. The most significant declines were in Medicaid expansion states where costs are less than half of the costs in non-expansion states.
How has structural racism contributed to health inequities?
Most of the 2 million Americans without expanded coverage live in eight states in the South, where the legacy of slavery persists.
In rural Black communities, people often lack adequate access to basic preventive health care services to treat chronic diseases, and many uninsured people avoid doctor’s visits until it’s a life-or-death scenario.
The pandemic has underscored how those inequities can be deadly. Earlier this year, we found that Black Americans were more likely than white people to test positive for COVID-19, almost four times as likely to be hospitalized and nearly three times as likely to die of the virus.
Help support this work
Public Integrity doesn’t have paywalls and doesn’t accept advertising so that our investigative reporting can have the widest possible impact on addressing inequality in the U.S. Our work is possible thanks to support from people like you. Donate now.
Read more in Inequality, Opportunity and Poverty
Inequality, Opportunity and Poverty
These books tackled inequality in 2021
A year of deep looks at discriminatory systems in government, education, policing, poverty and media.
Inequality, Opportunity and Poverty
Carol Anderson: The Second Amendment is anti-Black
The Kyle Rittenhouse verdict and Ahmaud Arbery trial illustrate the Second Amendment’s racist roots, says author Carol Anderson.

Join the conversation
Show Comments