Introduction
We held a Q&A live chat for with Kristen Lombardi in our Environmental Health Facebook group last week to dive deeper into her investigation into how a warming climate affects the spread of disease-bearing ticks in the United States, particularly in Maine and northeastern states. Here’s a summary of that conversation.
Q: Can you tell us what made you want to pursue this particular story looking at the effect of climate change on tick-borne illnesses?
A: This piece was conceived as the first story in a series on the human health impacts of climate change. I began to hear about the health effects of climate change from doctors or nurses or other health-care professionals last year, and, at first, I did a kind of double-take when hearing such talk. I had often read about climate change and its environmental impacts (rising sea levels, rising temperatures, intensifying hurricanes) but not many stories had made the connection between those environmental impacts and their impacts to our health, and our kids’ health.
I began to ask doctors about it and they mentioned that more and more physicians and health-care professionals were sounding the alarm. They pointed me to a 2016 federal report that really laid out the health impacts of climate change manifesting themselves today and in the future in this country. I mention that report in this piece.
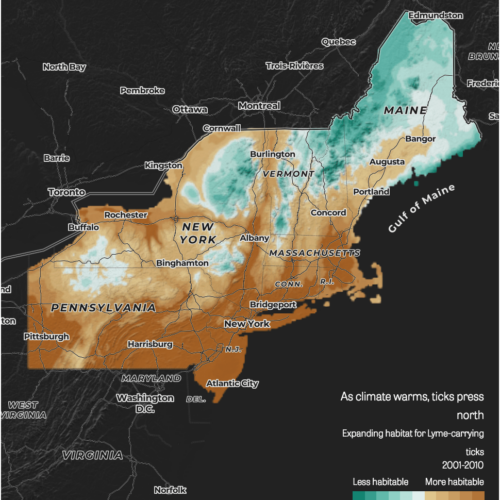
One of the health impacts is vector-borne diseases, including diseases caused by ticks and mosquitoes. I started looking at all vector-borne diseases but eventually gravitated toward tick-borne diseases. Scientists told me that of all infectious diseases, those caused by bites from mosquitoes, ticks and other cold-blooded insects are the most climate sensitive. Their range and distribution can be altered by just the slightest changes in temperatures.
Q: The story highlights Maine as a case study of this phenomenon. Can you talk about what was most revealing or significant in your reporting about what’s been happening in Maine relating to ticks?
A: For me, I started this piece by looking at Lyme and its link to climate change more broadly. I spoke with the CDC and other academic researchers who have been examining the influence of rising temperatures on the spread of Lyme first and almost all of them pointed to Maine as a dramatic example of this climate disease connection.
As my piece points out, there are other factors that drive the disease but scientists who have studied this link agree that climate is the primary driver in Lyme’s movement north. If you ask the scientists what constitutes the disease’s “northern margins,” they will name such states as Minnesota, the Upper Peninsula of Michigan, northern New York, New Hampshire and Vermont–states or northern areas of states where deer ticks and Lyme disease barely registered back in the 1990s, when the federal CDC began collecting Lyme data.
Most of those scientists note that Maine is about as north as you can get in this country and the changes in the distribution and range of the deer tick and incidence of Lyme disease are striking. Hearing this from the scientists I began looking at Maine’s Lyme incidence rate and it is skyrocketing. Federal data show Lyme disease cases have increased 20 fold. The state now leads the country in its incidence rate per capita.
Read the story: As disease-bearing ticks head north, weak government response threatens public health
Q: And as the article mentions, state plans to incorporate or acknowledge climate change as part of Maine’s public health response has been challenging?
A: Yes, that’s correct. One of the things we set out to do with this story and what we hope to do with the overall series is not just to connect the dots for people between climate-related health risks but to dig into the government’s response. The Maine CDC is among a group of states that is considered leading the nation in trying to tackle the health threats of climate change, because it has received a federal grant known as the Building Resilience to Climate’s Effects grant.
I assumed that the Maine CDC would want to talk about all the work it was doing related to this grant, but that was not the response I got. I began to learn more about the program in Maine, and I found out that it had started with rather ambitious plans that have yet to be carried out.
Part of its ambitious strategy would have helped the state get ahead of the tickborne disease epidemic there. We thought that what was happening in Maine might serve as a microcosm showing how difficult it is for state health departments to fully address this epidemic when politics around climate change come into play.
Q: Some readers of the story when it published wanted to know whether it was worth focusing on something as “political” as climate change as the best response to the disease epidemic. Were there other strategies the health departments are also trying to implement alongside the climate-related work?
A: Well, the point of this story was to examine that connection between vector-borne disease and climate change, just as it is important to examine that connection between heat-related conditions and climate change or pollen allergies and climate change or waterborne diseases and climate change (all health effects of climate change we were hoping to explore). It’s clear from my reporting that there are other factors that contribute to the spread of ticks and tick-borne diseases besides global warming. I mention in the piece how the federal Lyme data shows the disease spreading far beyond its historically endemic areas to places not just north but also south and west. Talking with scientists they suspect this changing land-use pattern is behind Lyme’s spread in mid-Atlantic states like Pennsylvania, Virginia, DC, Ohio, etc, where the incidence rate has really soared since the 1990s, for instance.
When talking with public health officials at the federal and state levels, they explained that there are strategies that have long existed that will help address the tick-borne disease epidemic today, such as Lyme prevention campaigns focused on personal protection measures and especially tick surveillance and tick control strategies.
Q: What would you say is a takeaway for readers of this story who don’t have any of these diseases and for those who do? What should they be aware of?
A: What I hope people take away from this piece is a new way of looking at perhaps an old disease–whether it’s Lyme or heat stroke or asthma or pollen allergies. These are all adverse health conditions that are going to be made worse by climate change, according to all the latest science. Climate change may not be causing these conditions but rising temperatures and extreme precipitation and other changing climate factors will make these adverse health conditions worse. Yet public health experts say our front-line defenders for public health–our local and state health departments–are woefully prepared to handle these public health impacts.
Part of that is because anything having to do with climate change, including how it will affect our health and our kids’ health and so on, has become so politicized that public health officials don’t have the resources to identify and prepare for these worsening impacts. Part of it is discord within the health community itself, with officials recognizing climate change but not seeing it as a public-health crisis. Most of the experts I interviewed believe that climate change is the biggest public health crisis facing us today, and that it has the potential to wipe away all public-health gains made over the past 50 years. I think just being aware of that climate health connection is perhaps the most important takeaway.
Read more in Environment
Environment
Blowout: Inside America’s Energy Gamble
While the U.S. produces more fossil fuels than ever and sells them to the rest of the world, climate change increasingly makes its presence known through heat waves, wildfires, droughts and floods.
Environment
Big Oil’s black mark on California’s climate record
The state’s oil regulator has the dual burden of facilitating oil development while protecting the environment and public health. Can it do both?

Join the conversation
Show Comments